Complete resolution for recurrence Triple-Negative Breast Cancer (TNBC), Stage IIB (pT2N1M0)
- JRX Global
- Oct 22, 2025
- 3 min read
Updated: Nov 10, 2025

Mrs. Lily Ngai Kuan Lay, a 58-year-old Malaysian female, first discovered a small lump in her left breast in May 2024. She had no previous history of similar symptoms, but her instinct told her to seek medical attention immediately. A mammogram and PET/CT scan soon revealed an irregular hypermetabolic nodule in her left breast and an enlarged left axillary lymph node, both showing high FDG uptake. The findings were consistent with malignancy, and the diagnosis confirmed Triple-Negative Breast Cancer (TNBC), Stage IIB (pT2N1M0), an aggressive subtype that does not express estrogen, progesterone, or HER2 receptors.
On 1 June 2024, she underwent a wide segmental excision of the tumour along with an axillary dissection, during which 18 lymph nodes were removed and one was found to contain metastatic cancer cells. Histopathology revealed a 3.3 cm invasive ductal carcinoma of grade 3, poorly differentiated, but with clear surgical margins.
Following surgery, Mrs. Ngai embarked on an intensive course of chemotherapy and radiotherapy between July and September 2024. She completed all cycles as scheduled, and her post-treatment PET/CT on 2 October 2024 brought encouraging news, there was no evidence of local tumour recurrence or distant metastasis. The results suggested a good initial response, and she looked forward to recovery.
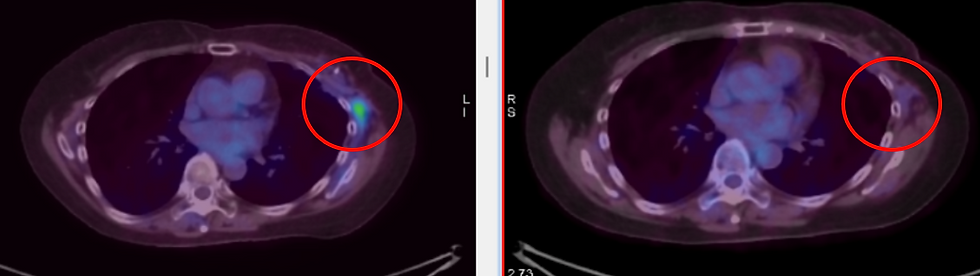
However, her journey took an unexpected turn in early 2025. A follow-up PET/CT on 6 March 2025 showed a diffuse increase in metabolic activity at the left axilla and chest wall and the appearance of a small mildly FDG-avid parasternal node. While these changes could have been post-treatment inflammation, her medical team decided to keep a close watch. Three months later, a PET/CT on 9 June 2025 revealed progression, the parasternal node had enlarged and two new FDG-avid mediastinal nodes had appeared. A biopsy confirmed metastatic poorly differentiated adenocarcinoma consistent with her primary breast cancer, indicating disease recurrence Triple-Negative Breast Cancer.
Despite the recurrence, Mrs. Ngai remained calm and determined. Having completed all standard treatments (surgery, radiotherapy, chemotherapy, and oral chemotherapy), she explored additional options to strengthen her fight. Her physical condition remained good; she was alert, active, and maintained her appetite and weight. The only persistent side effect was mild lymphatic swelling in her left arm, about one to two centimeters larger than the right, which improved with physiotherapy. Her blood results were mostly stable, showing only mild liver enzyme elevation. After discussions with ECCT team, she decided to start ECCT in June 2025 as a complementary treatment alongside her conventional care. She uses a therapeutic ECCT blanket and continued light supplementation and practiced physiotherapy to manage her swelling.
A few days upon started ECCT, further immunohistology testing revealed that her tumour expressed PD-L1 with a CPS score above 10, making her eligible for immunotherapy with durvalumab. This was combined with a new course of chemotherapy while maintaining ECCT sessions regularly. Through this phase, she remained disciplined and consistently even while balancing rest and family activities. ECCT medical team closely monitored her performance and adjust the regime when necessary.
Three months later, in October 2025, a repeat PET/CT scan brought truly remarkable news. All previously FDG-avid nodes including the parasternal and mediastinal lesions had completely resolved. There was no sign of local recurrence, no distant metastasis, and no abnormal metabolic activity. Her oncologist described the response as a very good outcome with the combination treatments.




Physiologically, Mrs. Ngai felt strong and energetic. She was able to perform her daily routines independently, with a good appetite and stable sleep. The only notable laboratory issue was mild anemia (Hb 8.7 g/dL), which improved after a single blood transfusion. Her liver function remained stable and she showed no symptoms of systemic inflammation or drug toxicity.
Today, Mrs. Ngai’s condition is described as complete metabolic remission. Her most recent PET/CT on 8 October 2025 confirmed that all metastatic nodes had resolved, and there was no evidence of active cancer.
Her journey from diagnosis to recovery has been defined by courage, discipline, and faith in treatment. Against the challenge of a highly aggressive form of breast cancer, Mrs. Ngai has shown that perseverance, supported by an integrative treatment strategy, can bring new hope and enhance treatment outcomes and quality of life, a shining example of strength and recovery in the face of adversity.



Comments