Stabilization of metastatic lung adenocarcinoma signet-ring type using ECCT
- Jun 1, 2025
- 3 min read
A 65-year-old female diagnosed with metastatic lung adenocarcinoma signet-ring type had undergone extensive multimodal treatment since 2020, including targeted therapy (crizotinib, lorlatinib), immunotherapy (OSEL), microwave ablation, and Gamma Knife radiosurgery for brain metastases. Despite partial responses, disease activity remained high—particularly in the oesophageal region, where biopsy confirmed metastasis from the lung primary.
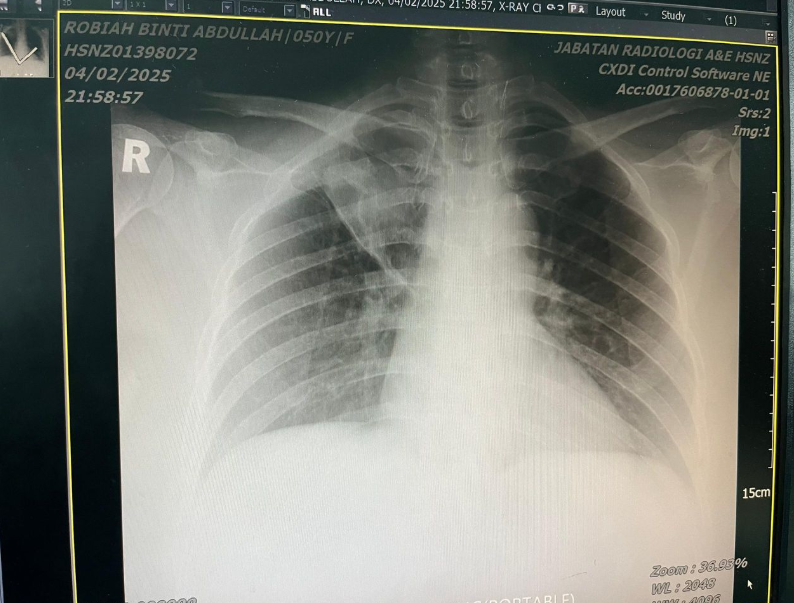
Before ECCT
The patient’s condition was deteriorating due to progressive tumour activity in the oesophagus and mediastinal lymph nodes.
- PET-CT (Mid-2024):
- Showed a large para-oesophageal lesion with intense FDG uptake.
- Disease considered progressive despite ongoing lorlatinib.
- Brain metastases (right temporal and cerebellar) had improved post–Gamma Knife, but systemic control was suboptimal.
- The patient had increasing difficulty swallowing, frequent choking episodes, and required repeated endoscopic interventions.
At this stage, the disease was active, metabolically aggressive, and symptomatic, with limited further systemic therapy options due to cumulative toxicities and organ sensitivity.
Start of ECCT
Given the limited conventional options and the need for tumour control, ECCT was initiated as an adjunct therapy. The objective was to suppress tumour metabolic activity, improve local control of the oesophageal lesion, and stabilise systemic disease without adding significant toxicity.
ECCT was applied in combination with continued targeted therapy and integrated supportive care. The patient tolerated ECCT well, with no major side effects apart from mild fatigue during the initial phase.

After ECCT
1. PET-CT (~6 months after ECCT start):
- Marked decrease in FDG uptake at the para-oesophageal site (Reduced from 10.1 → 7.5).
- No new metastases detected elsewhere.
- Brain lesions remained stable and inactive on MRI.
- Clinically, swallowing improved, food tolerance increased, and general energy levels were better maintained.
2. PET-CT (~9 months after ECCT start):
- Further reduction in metabolic activity.
- The previously aggressive oesophageal lesion appeared smaller and less active.
- No evidence of new visceral or bone metastases.
- Brain MRI confirmed continued regression of both the right temporal and cerebellar metastases, with minimal residual enhancement.
3. Clinical and Functional Progress:
- Swallowing improved significantly; the patient managed a semi-solid diet with fewer choking episodes.
- Systemic condition stable with preserved organ function and controlled symptoms.
- Fatigue and reflux were mild and manageable.
- Weight and nutritional status improved compared to pre-ECCT baseline.
Later follow-up CT imaging revealed a contained oesophageal leak and mild vertebral changes consistent with osteomyelitis, a complication secondary to stent placement—not tumour progression. Importantly, no systemic disease flare was detected, and tumour metabolic activity remained low.
The patient continued maintenance ECCT sessions and targeted therapy, with multidisciplinary monitoring. Overall, the disease was biologically quieter and metabolically less active compared to the pre-ECCT period.
Summary of Imaging Comparison (Before vs After ECCT)
Imaging Period | Key Findings | Oesophageal Site | Interpretation |
Before ECCT | Large active lesion, progressive disease | 14.3 | High metabolic activity, symptomatic |
~6 months ECCT | Reduced lesion uptake, no new metastases | 7.5 | Partial metabolic response |
~9 months ECCT | Further reduction, smaller lesion | 3.9 | Sustained regression, disease stabilisation |
Before ECCT, the patient’s cancer was active and symptomatic despite years of targeted and local therapies. After incorporating ECCT, sequential imaging demonstrated steady reduction in tumour metabolic activity, no new metastatic spread, and improved clinical well-being.
The overall evidence suggests that ECCT contributed meaningfully to suppressing disease activity, stabilising progression, and enhancing the patient’s quality of life in a setting where conventional options had reached their limits.


Comments